| Connect & Subscribe |
Hypopnea Brochure
An Outreach Project by Jane Yoon | Return To Outreach Projects 2010
The following is a brochure created for Stanford Sleep and Dreams. If it is difficult to read using the images, you may view the text here.
Also feel free to download this brochure for distributional or general information purposes. Please refer to our privacy policy for our relevant disclaimers.
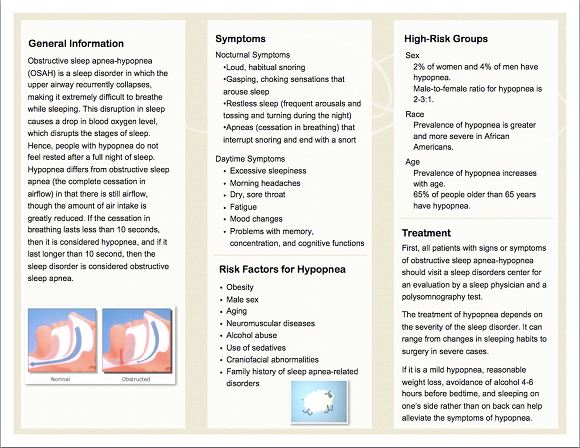
General Information
Obstructive sleep apnea-hypopnea (OSAH) is a sleep disorder in which the upper airway recurrently collapses, making it extremely difficult to breathe while sleeping. This disruption in sleep causes a drop in blood oxygen level, which disrupts the stages of sleep. Hence, people with hypopnea do not feel rested after a full night of sleep. Hypopnea differs from obstructive sleep apnea (the complete cessation in airflow) in that there is still airflow, though the amount of air intake is greatly reduced. If the cessation in breathing lasts less than 10 seconds, then it is considered hypopnea, and if it last longer than 10 second, then the sleep disorder is considered obstructive sleep apnea.
Symptoms
Nocturnal Symptoms
Daytime Symptoms
Risk Factors for Hypopnea
Obesity
High-Risk Groups
Sex - 2% of women and 4% of men have hypopnea.Male-to-female ratio for hypopnea is 2-3:1.
Race - Prevalence of hypopnea is greater and more severe in African Americans.
Age- Prevalence of hypopnea increases with age.65% of people older than 65 years have hypopnea.
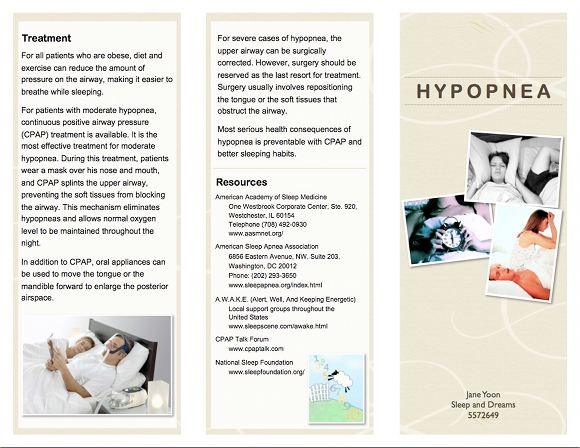
Treatment
First, all patients with signs or symptoms of obstructive sleep apnea-hypopnea should visit a sleep disorders center for an evaluation by a sleep physician and a polysomnography test.
The treatment of hypopnea depends on the severity of the sleep disorder. It can range from changes in sleeping habits to surgery in severe cases.
If it is a mild hypopnea, reasonable weight loss, avoidance of alcohol 4-6 hours before bedtime, and sleeping on one's side rather than on back can help alleviate the symptoms of hypopnea.
For all patients who are obese, diet and exercise can reduce the amount of pressure on the airway, making it easier to breathe while sleeping.
For patients with moderate hypopnea, continuous positive airway pressure (CPAP) treatment is available. It is the most effective treatment for moderate hypopnea. During this treatment, patients wear a mask over his nose and mouth, and CPAP splints the upper airway, preventing the soft tissues from blocking the airway. This mechanism eliminates hypopneas and allows normal oxygen level to be maintained throughout the night.
In addition to CPAP, oral appliances can be used to move the tongue or the mandible forward to enlarge the posterior airspace.
For severe cases of hypopnea, the upper airway can be surgically corrected. However, surgery should be reserved as the last resort for treatment. Surgery usually involves repositioning the tongue or the soft tissues that obstruct the airway.
Most serious health consequences of hypopnea is preventable with CPAP and better sleeping habits.
Resources
American Academy of Sleep Medicine One Westbrook Corporate Center, Ste. 920, Westchester, IL 60154 Telephone (708) 492-0930 www.aasmnet.org/
American Sleep Apnea Association 6856 Eastern Avenue, NW, Suite 203, Washington, DC 20012 Phone: (202) 293-3650 www.sleepapnea.org/index.html
A.W.A.K.E. (Alert, Well, And Keeping Energetic) Local support groups throughout the United States www.sleepscene.com/awake.html
CPAP Talk Forum www.cpaptalk.com
National Sleep Foundation www.sleepfoundation.org
About This Site
Welcome! This site is continuously being created by students of Dr. William C. Dement's Sleep And Dreams course at Stanford University.
We made this site as a call to action for people all over the world to live healthier, happier, safer, and more productive lives by learning about their own sleep. We have faith that reading the information provided on this site will motivate you to be smart about your sleep deprivation and strategic about your alertness in order to live life to your fullest, most energetic potential.
In fact, we challenge you to do so! What do you say, are you up for the challenge?
Interviews With Sleep Specialists: Insights Into the Worlds of Sleep Medicine & Sleep Business
America's Most Dangerous Disorder: What Is Sleep Apnea Doing To Your Sleep?
Sleep Debt: How Much More Will You Achieve When You Reduce Yours?
The Stages Of Sleep: The Journey Through The Night
Delayed Sleep Phase: You Want To Sleep But You're Not Tired Yet
Paralyzed at Night: Is Sleep Paralysis Normal?
Sleep In Words: Smart, Strange, and Funny Quotes About Sleep
Sleep Disorders In Children: What's Keeping Your Child From A Full Night's Rest?
Attacks of Pavor Nocturnus (a.k.a. Sleep Terrors, Night Terrors, or Incubus Attacks)
The Stanford Sleep Book
Dr. Dement's pioneering textbook has been the core text for Sleep and Dreams since 1980, but it has just recently been made available to the wider public for the first time.
In it you'll find a more detailed account of the most important things you need to know about sleep, alertness, dreams, and sleep disorders. Studies, statistics, plus plenty of Dr. Dement's classic anecdotes painting the history of sleep medicine.
Preface | Intro | Contents | Get A Copy
More Sleep Resources
The Zeo
A revolution in personal sleep tracking, the Zeo is a wireless headband that transmits your brainwaves in realtime to a dock (pictured here) or your smartphone. The result? You can wake up and see exactly what stages of sleep you were in during the night! Unprecedented personalized sleep knowledge.
Sleep Paralysis: A Dreamer's Guide
Ever woken up paralyzed? A surprising number of us have, believe it or not. But few know the actual causes of this phenomenon, and fewer still how to exert control over it. Dream researcher and sleep paralysis expert Ryan Hurd shares breakthrough insights into how to do just that.
Important Disclaimer
Please Note:
The information found on this page and throughout this site is intended for general information purposes only. While it may prove useful and empowering, it is NOT intended as a substitute for the expertise and judgments of healthcare practitioners.
For more info, see our
Terms of Use.